Bone Densitometry
Make an Appointment
Call 413-794-2222A bone densitometry test determines the strength of your bones and your risk for breaking a bone.
If you have bone density loss (osteopenia) or osteoporosis, you could be at risk for painful bone fractures. To determine your risk of a fracture before one occurs, your physician may recommend that you undergo a bone densitometry test – also called bone density scanning or dual-energy X-ray absorptiometry (DXA).
Our experienced radiologists use an advanced, state-of-the-art bone densitometry system to accurately measure the bone mineral density (BMD) in your spine, hip or wrist in exceptional detail.
The test can also detect existing vertebral compression fractures (when the bones in your spine weaken and collapse), which helps us to determine your risk of future fractures.
The exam is painless, quick, and noninvasive; does not require anesthesia; and uses less radiation than a standard chest X-ray.
Who is a candidate for bone densitometry?
Millions of men and women are at risk for osteoporosis as they age because of calcium loss and structural changes that cause the bones to become thinner and weaker. Women in particular are susceptible to bone loss.
You may need a bone densitometry test if you are at risk for bone loss and fractures.
Risk factors for bone loss and fractures include:
Age: Women over 65 and men over 70 are at increased risk.
- Fragility fractures: These are bone fractures that occur after falling from standing height or lower. Most falls from standing height or lower do not result in fractures, so if you develop a fracture after this type of fall, you may have significant bone weakness.
- Medications: Anti-inflammatory treatments for certain conditions, including chronic lung disease, rheumatoid arthritis, Crohn's disease and asthma, can lead to weaker bones.
- Discontinued estrogen use: If you have recently stopped using estrogen therapy, you may be at increased risk.
- History of fracture: If you have a history of bone fractures, you may need a bone densitometry test.
- Low body weight: This means you are underweight for your height and could indicate bone density loss.
Note that the bone densitometry exam may not be effective if you have a spinal deformity or have had spine surgery.
How to prepare for a bone densitometry exam
On exam day, you should:
- Eat as you normally would, but refrain from taking calcium supplements for at least 24 hours prior to your exam.
- Wear comfortable, loose-fitting clothing.
- Avoid wearing clothing or accessories with metal buttons, zippers, or belts.
- Let your doctor know if you have been injected with contrast material for a computed tomography (CT) scan or nuclear medicine scan, if you have recently had a barium exam, or if you could be pregnant.
What to expect during a bone densitometry exam
During the test, your radiologist will use a DXA machine to send an invisible, thin beam of low-dose X-rays through your bones. Your soft tissues will absorb the first beam, and then your bones will absorb the second beam. Your radiologist will calculate your bone mineral density score by subtracting your soft tissue amount from the total amount. This determines the strength of your bones.
Here is what to expect during the 10- to 20-minute exam:
- You will be asked to remove your eyeglasses, any metal objects, and jewelry.
- You will lie on a padded table with an X-ray generator below you and an imaging device above you.
- Your legs will be supported on a padded box during the spine assessment.
- Your foot will be placed in a brace during the hip assessment.
- The imaging device will pass over you slowly as it generates images on a computer monitor.
Once your radiologist has completed the bone densitometry test, your referring physician, such as your primary care doctor, will receive a detailed report of your results.
Vertebral (spine) fracture assessment
Using the same DXA machine and technology used during a bone densitometry test, your radiologist can perform a vertebral fracture assessment (VFA) to determine if your spine has any fractures.
Who is a candidate for vertebral fracture assessment?
Talk to your doctor about VFA if you fall into one of the following categories:
With low bone density, as well as at least one of the following risk factors for spine fracture:
- Age 70 or older
- Previous height loss of 1.6 inches or more
- Your physician has predicted a future height loss of 0.8 inches or more
- Previous vertebral fracture
- Age 60 to 69
- Previous non-vertebral fracture
- Previous height loss of 0.8 to 1.6 inches
- Chronic disease associated with increased risk of fracture, including chronic obstructive pulmonary disease (COPD), chronic obstructive airways disease, Crohn's disease or seropositive rheumatoid arthritis
And one of the following risk factors for spine fracture:
- Age 80 or older
- Previous height loss of more than 2.4 inches
- Your physician has predicted a future height loss of more than 1.2 inches
- Self-reported non-vertebral fracture
And two or more of the following risk factors:
- Age 70 to 79
- Self-reported non-vertebral fracture
- Previous height loss of 1.2 to 2.4 inches
- On pharmacologic androgen deprivation therapy
- One or both testicles have been removed
- Chronic disease associated with increased risk of fracture, including chronic obstructive pulmonary disease (COPD), chronic obstructive airways disease, Crohn's disease or seropositive rheumatoid arthritis
- On chronic glucocorticoid therapy (5 milligrams or more of prednisone daily for three months or more)
- Osteoporosis and documentation of at least one vertebral fracture

View your radiology results online
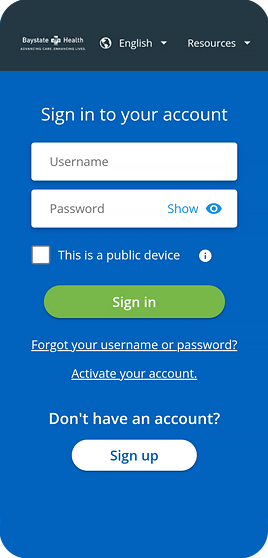
Your Health Record, the Way You Want it
Get Started
Back to Top

