Diabetes Management: Our Tips to Thrive with Diabetes
This article was reviewed by our Baystate Health team to ensure medical accuracy.
 Cecilia A. Lozier, MD
View Profile
Cecilia A. Lozier, MD
View Profile
Where should my levels be with diabetes?
Dr. Lozier emphasizes that these targets are generalized targets. “If you have diabetes, it’s important to work with your doctor and other specialists to establish what levels are best for you based on how your body metabolizes carbohydrates.”
Other Approaches to Controlling Diabetes
Beyond monitoring your A1C and sugar levels, Dr. Lozier notes there are other things you can do to stay on top—and even ahead—of your diabetes.
Assuming you have no abnormal medical issues that require more frequent monitoring, she recommends annual screenings of the:
- Eyes
- Feet
- Blood and urine
- Blood pressure
- Cholesterol
- Gums through dental exams
“These screenings can reveal if any damage is taking place throughout the body and allow your doctors to make changes to how your diabetes is being treated to minimize future damage and allow you to live your best life as long as possible.”
She notes that high blood pressure, cholesterol, and smoking all have the potential to affect blood vessels as does diabetes. “To stay healthy, you need healthy blood vessels, so you really need to keep on top of any conditions that impact them. One condition isn’t good, but three or four is really bad news for your blood vessels.”
She adds there are also protective medications that work to protect organs in the body from damage that diabetes might cause. Currently, there are five classes of medications that may be prescribed and it’s important to talk with your provider to determine if you would benefit from adding them to your regimen.
Get Help with Your Diabetes Management
Because diabetes and blood sugar levels are an ever-moving target, it’s not uncommon for patients to need help managing their condition. Dr. Lozier encourages patients to reach out to their various providers when the following issues occur:
| Issue | Who to Contact |
|---|---|
| Sugar levels are above target range or not improving with lifestyle or medication change | Primary Care Doctor |
| You need help planning lifestyle changes or want to further explore how to lead a fulfilling, healthy life with diabetes | Certified Diabetes Care and Education Specialist (CDCES) |
|
You have type 1 diabetes, type 2 diabetes with A1C>9 despite insulin, or type 2 diabetes with A1C and the following:
|
Endocrinologist |
Diabetes Management Webinar


Health & Wellness Tips
Related Articles
-
Wellness & Prevention
![What are Different Types of Breast Cancer_ Plus Treatment Options]()
What are Different Types of Breast Cancer? Plus Treatment Options
-
Wellness & Prevention
![10 Breast Cancer Prevention Tips]()
Breast Cancer Prevention Myths and Facts from the Experts
-
Wellness & Prevention
![When to Get a Flu Shot]()
When to Get a Flu Shot This Year: What Experts Recommend
-
Wellness & Prevention
![a large lightning bolt striking from a dark sky during a severe thunderstorm]()
Storm Safety: Tips for Protecting Your Family and Home
-
Your Healthcare
![Woman pharmacist behind pharmacy counter, providing male patient with their medication.]()
Medication Safety: How Pharmacists Help You Manage Your Meds
-
Wellness & Prevention
![Over-the-Counter Birth Control Pills-What You Need to Know]()
Over-the-Counter Birth Control Pills: What You Need to Know
-
Coping with Illness
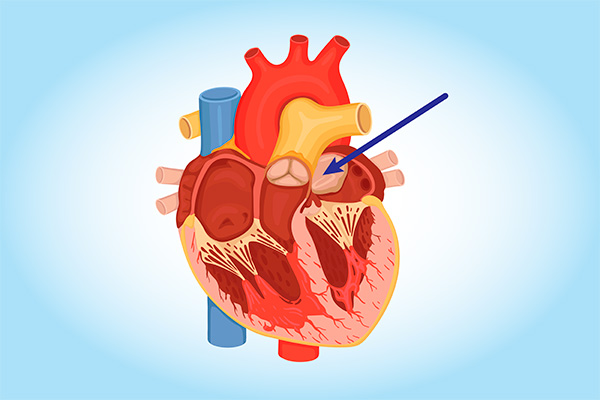
![cardiac myxoma heart tumor diagram]()
Can You Get Heart Cancer? It's Rare, but Yes. Learn the Symptoms
-
Wellness & Prevention
![Make your 2023 New Years Resolutions]()
5 Achievable 2024 Health-Related New Year's Resolutions
-
Wellness & Prevention
![feet in socks by a winter fire]()
Health Tips for the Holidays: Strategies to Stay Fit and Jolly
-
Wellness & Prevention
![a woman discussing pancreatic cysts with her doctor, waiting for an MRI scan]()
Are Pancreatic Cysts Dangerous? Do They Cause Pancreatic Cancer?
Back to Top