New Alzheimer's Disease Drugs Receive FDA Approval, Offering Hope
July 11, 2024
This article was reviewed by our Baystate Health team to ensure medical accuracy.
 Stephen J. Bonasera, MD
View Profile
Stephen J. Bonasera, MD
View Profile

Health & Wellness Tips
Related Articles
-
Wellness & Prevention
![What are Different Types of Breast Cancer_ Plus Treatment Options]()
What are Different Types of Breast Cancer? Plus Treatment Options
-
Wellness & Prevention
![When to Get a Flu Shot]()
When to Get a Flu Shot This Year: What Experts Recommend
-
Your Healthcare
![Woman provider speaking with patient while sitting at table.]()
Diagnosing and Treating Colon Polyps: What You Need to Know
-
Your Healthcare
![Woman pharmacist behind pharmacy counter, providing male patient with their medication.]()
Medication Safety: How Pharmacists Help You Manage Your Meds
-
Your Healthcare
![A smiling couple staring into each others eyes. The woman is laying on a bed, while the man is above her, with his face close to hers.]()
Navigating Low Libido: Insights & Solutions for Women
-
Your Healthcare
![an older Black man jogging in a park wearing headphones]()
Discover the Heart-Health Benefits of Weight Loss Medications
-
Coping with Illness
![surgeons in operating room performing heart bypass surgery]()
What is Heart Bypass Surgery? CABG Surgery Can Be a Lifesaver
-
Your Healthcare
![cardiac catheterization]()
Cardiac Cath Lab: Pioneering Non-Surgical Heart Solutions
-
Coping with Illness
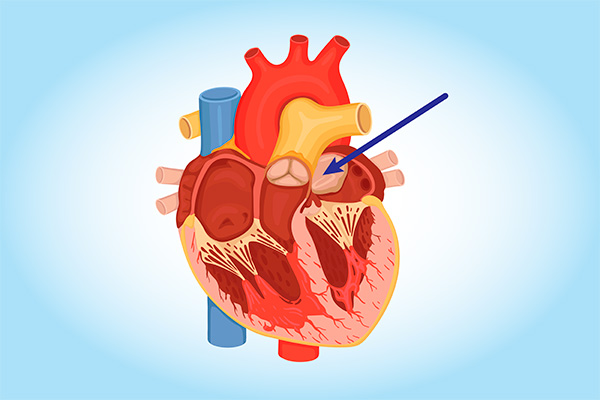
![cardiac myxoma heart tumor diagram]()
Can You Get Heart Cancer? It's Rare, but Yes. Learn the Symptoms
-
Wellness & Prevention
![Make your 2023 New Years Resolutions]()
5 Achievable 2024 Health-Related New Year's Resolutions
Back to Top