How to Win the Bedtime Battle: How-To Guide for Caregivers
September 12, 2024

Health & Wellness Tips
Related Articles
-
Wellness & Prevention
![What are Different Types of Breast Cancer_ Plus Treatment Options]()
What are Different Types of Breast Cancer? Plus Treatment Options
-
Wellness & Prevention
![10 Breast Cancer Prevention Tips]()
Breast Cancer Prevention Myths and Facts from the Experts
-
Wellness & Prevention
![When to Get a Flu Shot]()
When to Get a Flu Shot This Year: What Experts Recommend
-
Wellness & Prevention
![a large lightning bolt striking from a dark sky during a severe thunderstorm]()
Storm Safety: Tips for Protecting Your Family and Home
-
Your Healthcare
![Woman pharmacist behind pharmacy counter, providing male patient with their medication.]()
Medication Safety: How Pharmacists Help You Manage Your Meds
-
Wellness & Prevention
![Over-the-Counter Birth Control Pills-What You Need to Know]()
Over-the-Counter Birth Control Pills: What You Need to Know
-
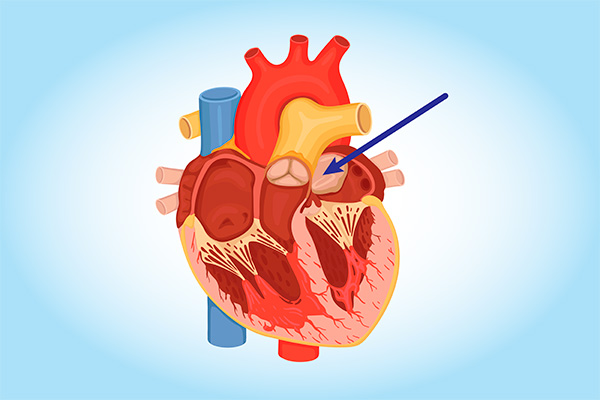
Coping with Illness
![cardiac myxoma heart tumor diagram]()
Can You Get Heart Cancer? It's Rare, but Yes. Learn the Symptoms
-
Wellness & Prevention
![Make your 2023 New Years Resolutions]()
5 Achievable 2024 Health-Related New Year's Resolutions
-
Wellness & Prevention
![feet in socks by a winter fire]()
Health Tips for the Holidays: Strategies to Stay Fit and Jolly
-
Wellness & Prevention
![a woman discussing pancreatic cysts with her doctor, waiting for an MRI scan]()
Are Pancreatic Cysts Dangerous? Do They Cause Pancreatic Cancer?
Back to Top